Treatment
Information
1 Benign Prostatic Hyperplasia A condition in which the prostate enlarges, causing various urinary symptoms.

Endovascular Treatment for
Benign Prostatatic Hyperplasia
Prostatic Artery Embolization
What is PAE?
Prostatic arterial embolization (PAE) as a new endovascular treatment for benign prostatic hyperplasia (BPH) has been gaining popularity, especially in Western countries. Although it is a relatively new treatment method, with the first reports of its efficacy appearing in the early 2000s, the initial case that drew attention to PAE as a treatment for BPH involved its use for controlling bleeding after a prostate tissue biopsy. Not only did PAE successfully achieve hemostasis, but it also improved symptoms of urinary difficulty associated with BPH, leading to its recognition as a potential treatment option.
Normal Prostate
Enlarged Prostate
【What is Benign Prostatic Hyperplasia (BPH)?】
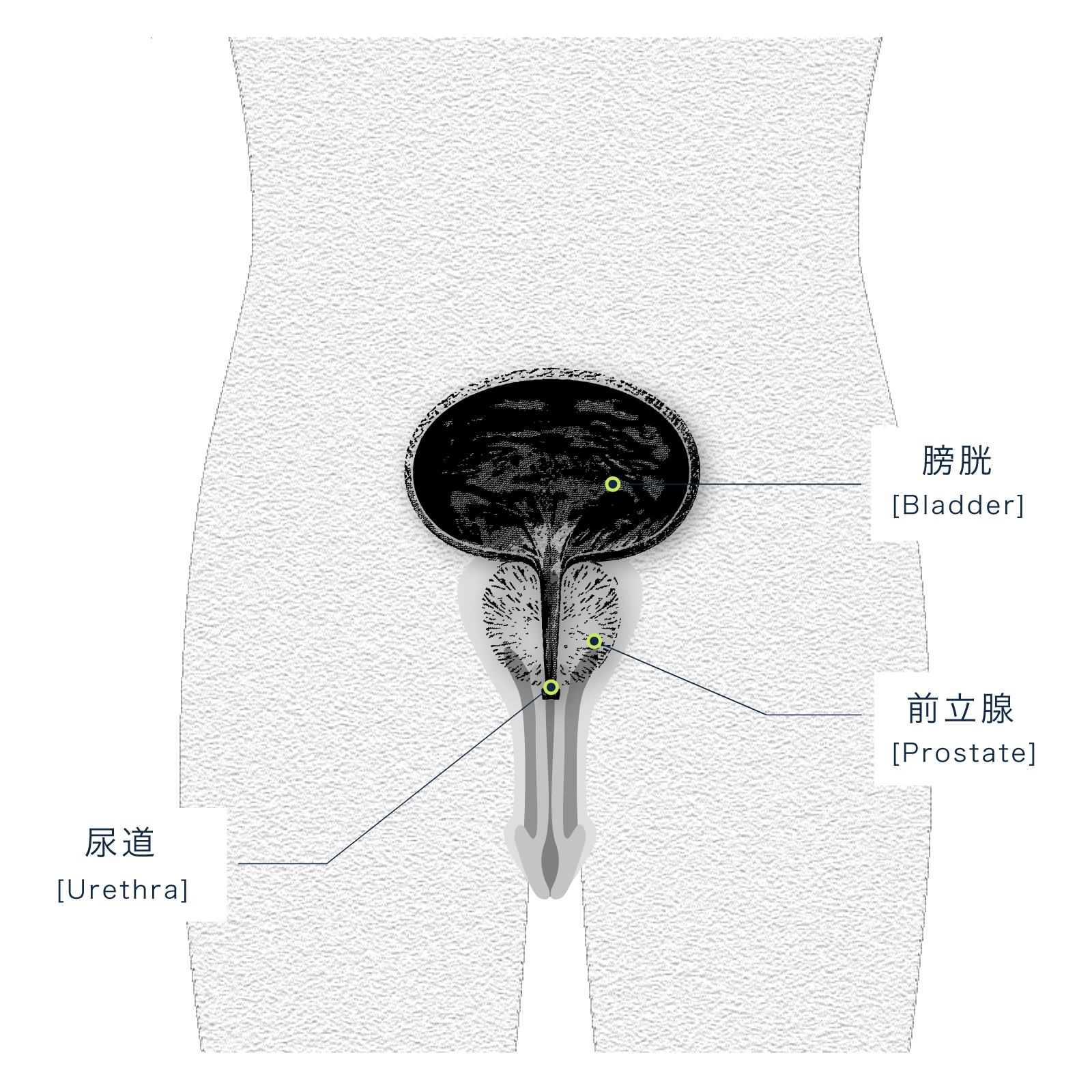
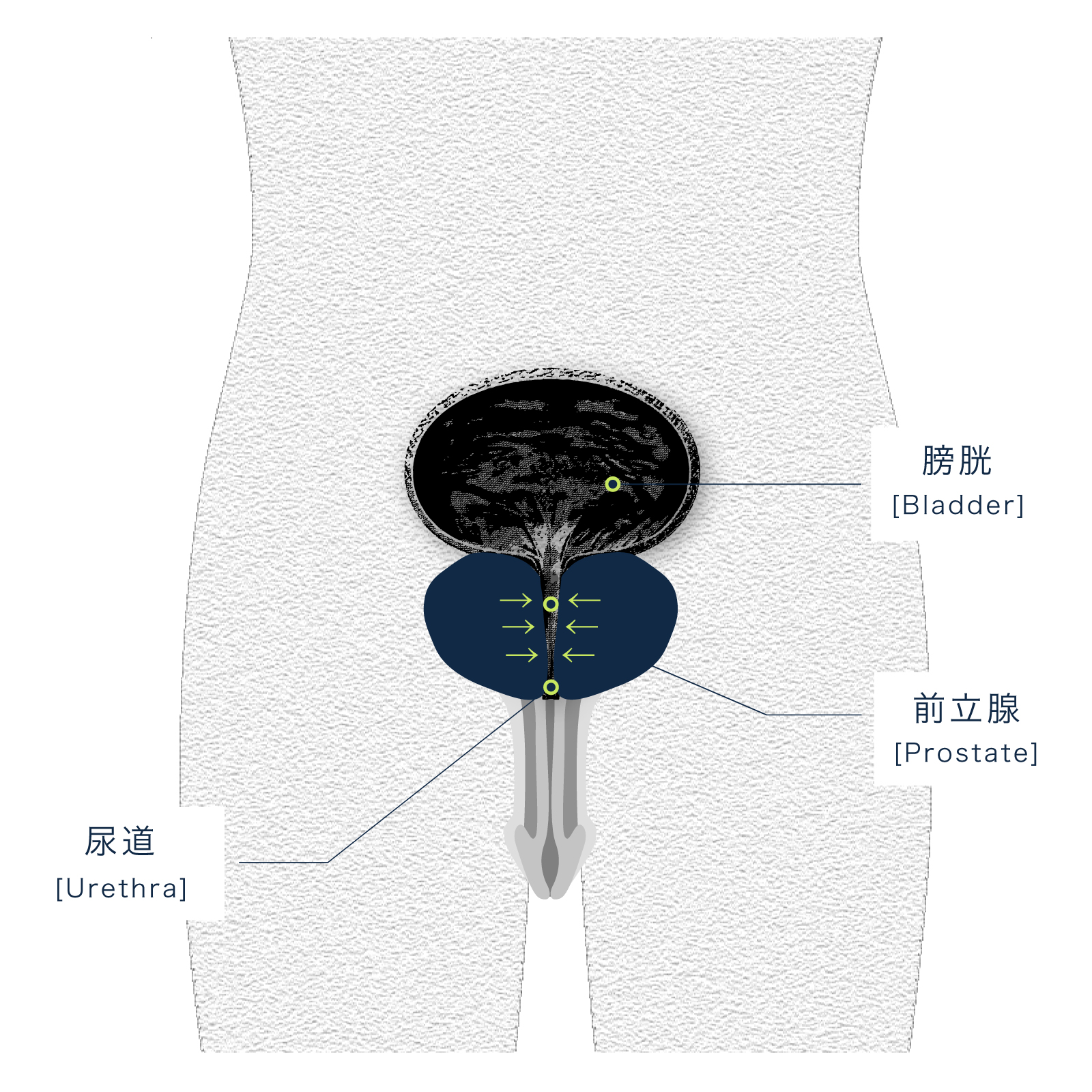
The prostate is an organ that exists only in men. In the average adult male, the prostate is typically less than 20 ml in size and is often compared to the size of a walnut. It is located at the outlet of the bladder, surrounding the urethra. Benign prostatic hyperplasia (BPH) is a condition in which the prostate enlarges, causing various urinary symptoms. The primary risk factor for BPH is aging; however, other factors such as genetics, diet, obesity, high blood pressure, high blood sugar, and dyslipidemia have also been reported. As the prostate enlarges, it can compress the urethra, leading to symptoms mainly related to urination, including voiding symptoms (such as difficulty urinating), storage symptoms (related to the bladder’s ability to hold urine), and post-micturition symptoms (symptoms that appear after urination).
【Main Symptoms】
[Voiding Symptoms]
Difficulty urinating, also known as voiding difficulty, is a general term for symptoms related to trouble with urination. These symptoms include “weak urine stream,” “difficulty starting urination even when you feel the urge,” “interruption of urine flow during urination,” and “the need to strain to urinate.
[Storage Symptoms]
In many cases of benign prostatic hyperplasia (BPH), frequent urination is observed. If you need to urinate more than approximately eight times between waking up in the morning and going to bed at night, it is considered “daytime frequency.” If you wake up to urinate more than once after going to bed at night, it is considered “nocturnal frequency.
[Post-Micturition Symptoms]
After urination, many people with benign prostatic hyperplasia (BPH) often complain of a feeling that “something doesn’t feel right” or “it feels like there’s still urine left,” known as a “sense of incomplete emptying.” Additionally, even after finishing urination, they may experience urine leakage that soils their underwear after putting it back on.
Treatment
The treatment for benign prostatic hyperplasia (BPH) typically begins with medication therapy. If the symptoms do not improve sufficiently with medication, surgical procedures like TURP (transurethral resection of the prostate) are considered. Prostatic arterial embolization (PAE), is a minimally invasive endovascular treatment and is widely used in Western countries for patients who do not respond adequately to medication therapy. Below, we present a table comparing the most common treatment options. While other surgical treatments are performed under general or spinal anesthesia, PAE is conducted under local anesthesia. Additionally, the hospital stay is typically short, often within two days, and in many hospitals, PAE is even performed as an outpatient procedure.

Methods of Prostatic Arterial Embolization (PAE)
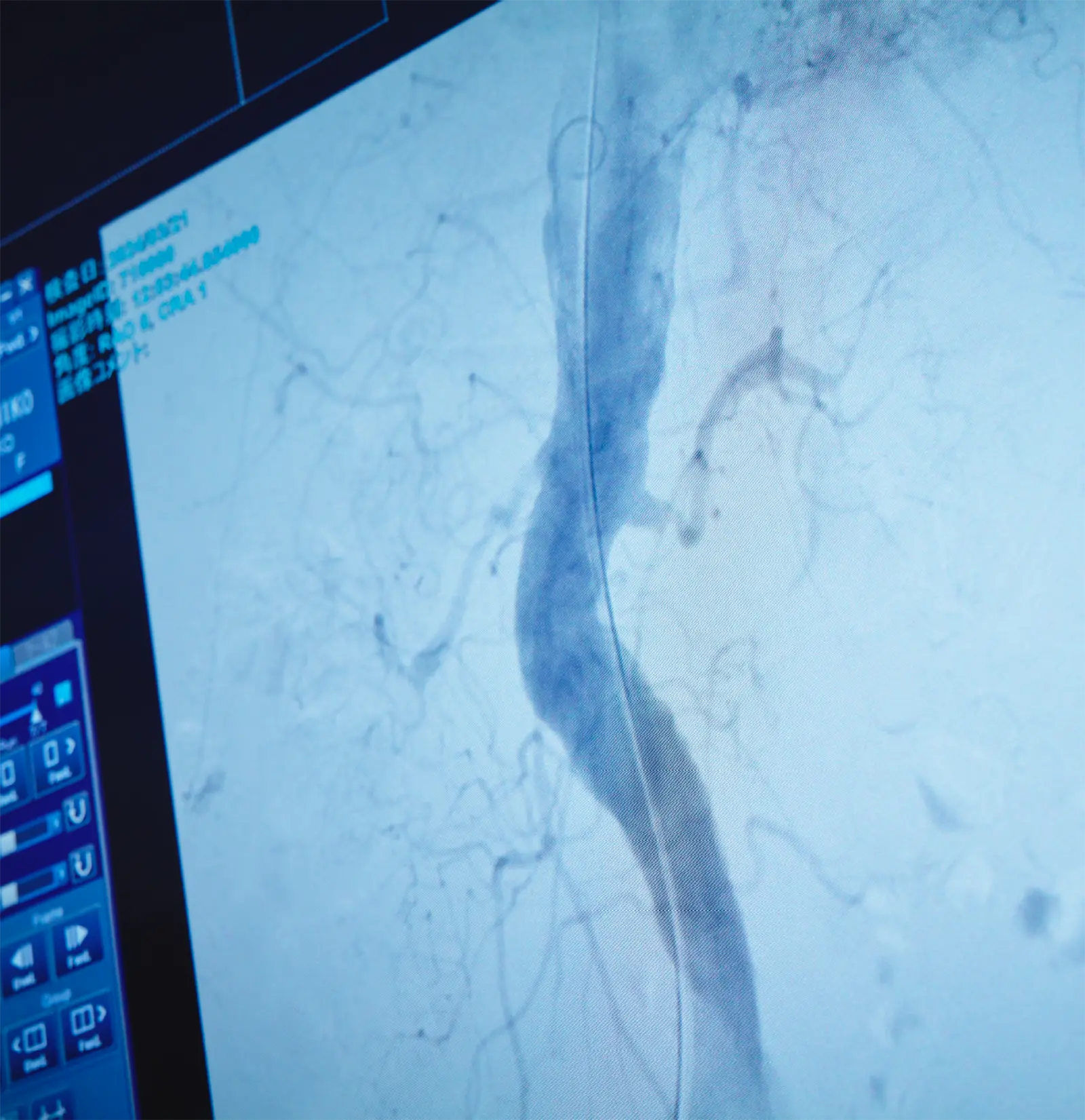
Puncture is performed under local anesthesia at either the common femoral artery in the groin or the radial artery in the wrist, and a catheter is inserted into both prostatic arteries for angiography.
Selective embolization material is injected into the prostatic arteries, blocking arterial blood flow to the prostate and inducing ischemia (a state in which the prostate does not receive nutrients). The prostate gradually undergoes necrosis and shrinks, leading to symptom relief.
Since this is a minimally invasive treatment, it can be performed on elderly patients or those with multiple comorbidities who are unable to undergo general anesthesia. Additionally, complications such as retrograde ejaculation, erectile dysfunction, and urethral stricture, which are known to occur after TURP and other surgeries, are less likely to occur with this procedure.
[Technical Success Rate and Therapeutic Efficacy]
It has been reported that in approximately 91-93% of cases, it is possible to successfully insert the catheter into bilateral prostatic arteries and inject embolic agents1,2. However, in about 7-9% of cases, due to arterial tortuosity, stenosis, or occlusion, the catheter cannot be advanced into bilateral prostatic arteries, resulting in embolization of only one side.
The recurrence rate of symptoms after PAE is approximately 11% at 12 months and about 20% at 30 months1. The rate at which PAE was repeated for recurrent symptoms is reported to be 3% at 1 year, 21% at 5 years, and 23% at 10 years2. Unlike traditional surgery, PAE is a endovascular treatment, making reintervention relatively easy to perform.
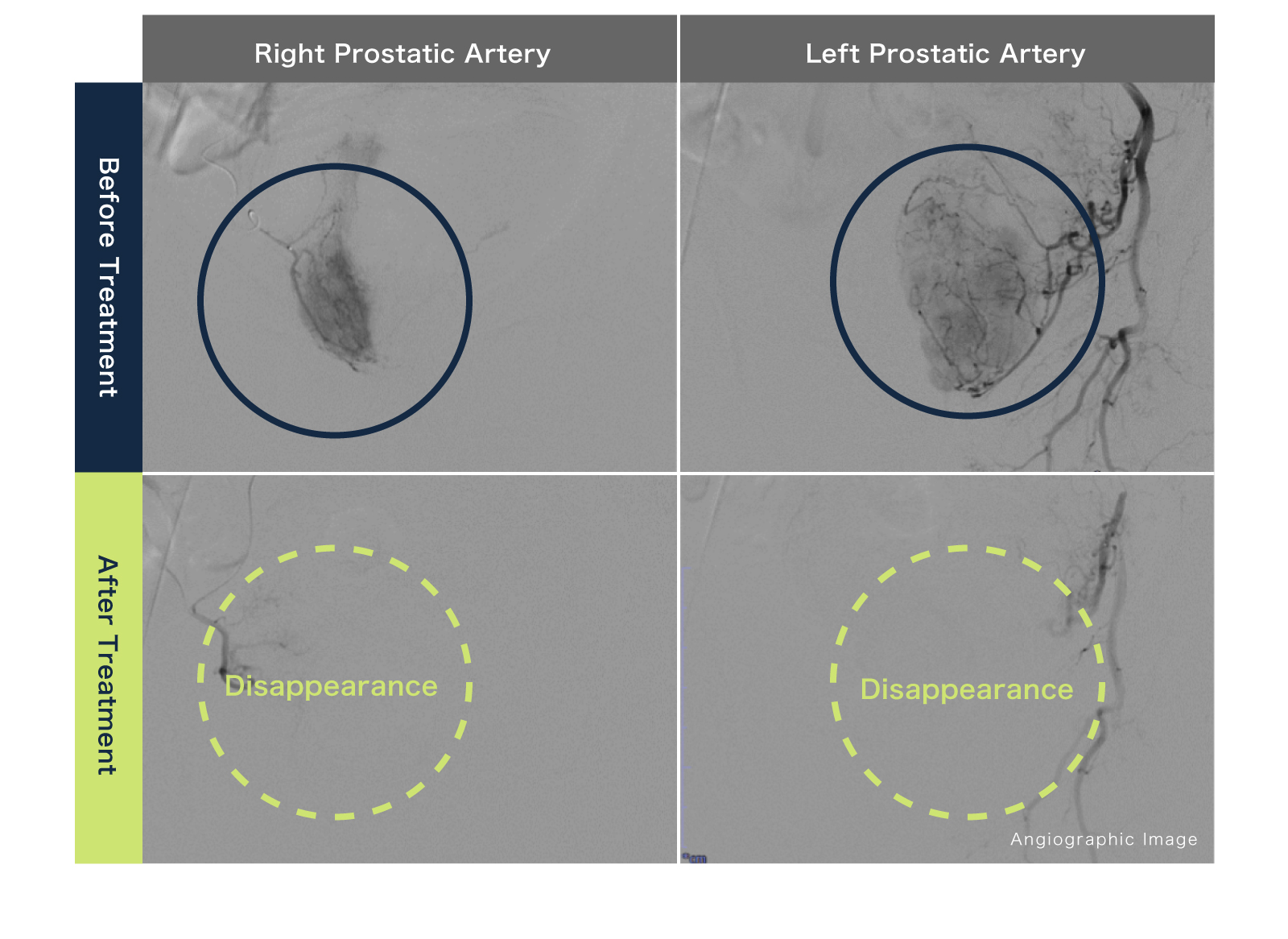
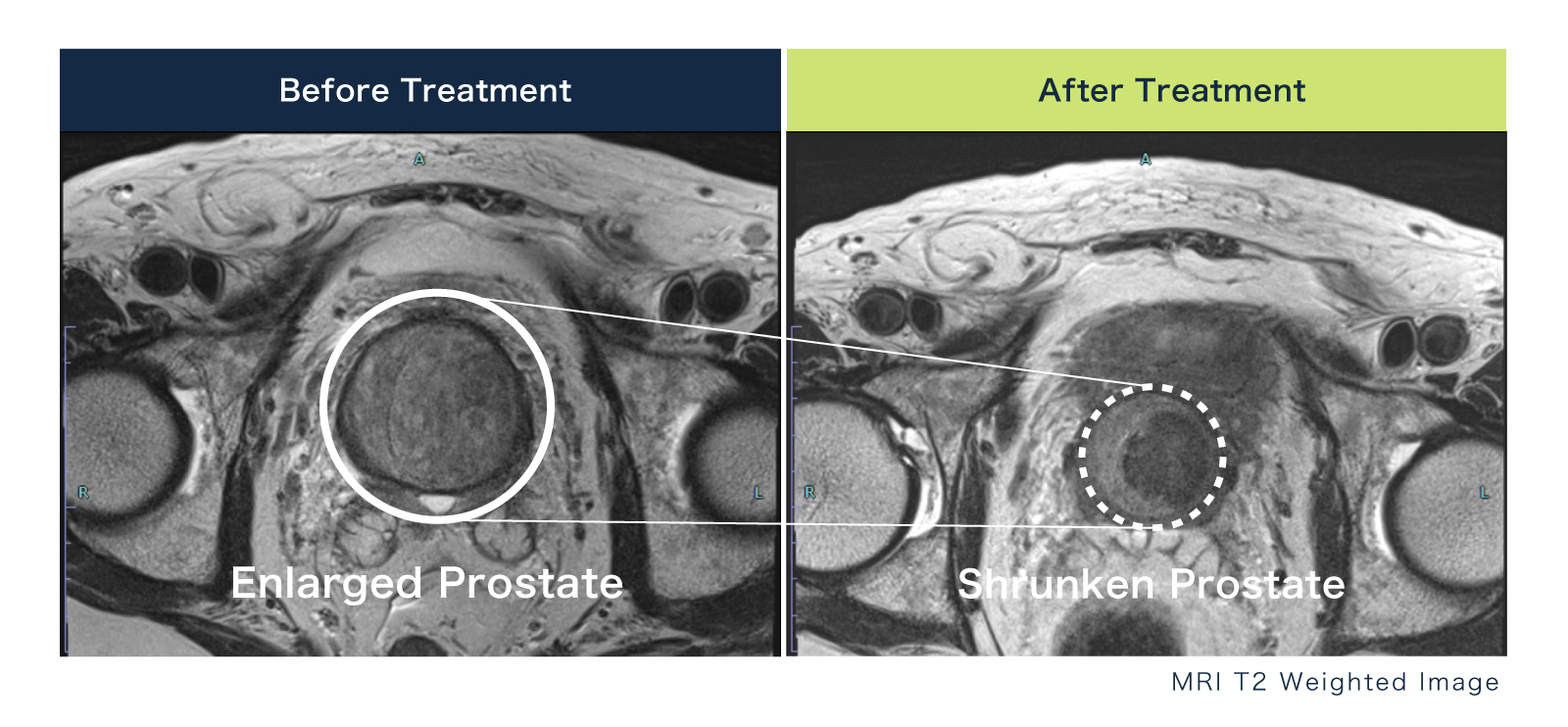
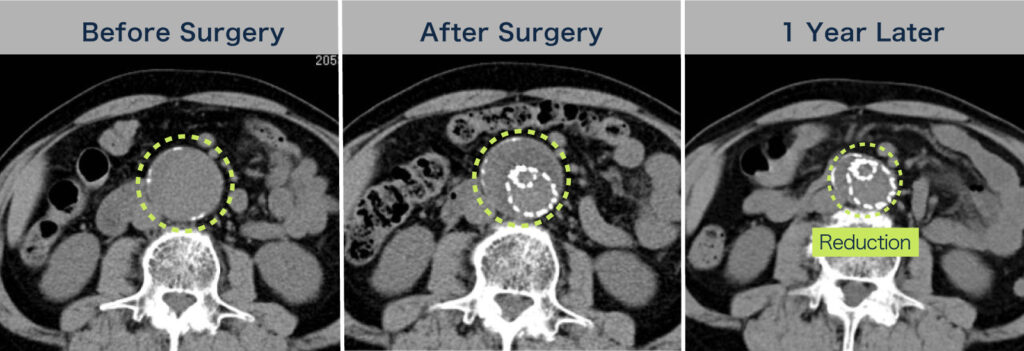
[Case Example]
The catheter was advanced into the prostatic arteries on both sides, and embolic agents were injected into each artery. Post-embolization angiography showed that the prostate was no longer visible, indicating successful blockage of blood flow. When comparing pre- and post-procedure MRI scans, significant shrinkage of the prostate is observed after the procedure. Before treatment, the patient needed to self-catheterize 4-5 times daily, but following PAE, self-catheterization is no longer necessary, and the patient is satisfied with the outcome.
[Complications of PAE]
PAE is reported to be a safe treatment with severe complications being rare. The complications that can occur are primarily related to embolic agents unintentionally flowing into vessels other than the prostatic arteries, which can result in issues such as penile ulcers, bladder ulcers, and rectal ulcers. Other potential complications include urinary tract infections, urinary retention, and vascular injury.
[Cost of Prostatic Artery Embolization (PAE)]
PAE is widely practiced in Western countries, but in Japan, it is a newly introduced medical procedure that has not yet been covered by insurance, making it a self-pay treatment. For details regarding the cost, please check with the medical institutions that offer PAE.
References:
- 1.Carnevale FC, Moreira AM, de Assis AM, et al. Radiology. 2020;296:444-51.
- 2.Bilhim T, Costa NV, Torres D, et al. Cardiovascular and interventional radiology. 2022;45:1324-36.
[Comparison of Treatment Options for Benign Prostatic Hyperplasia (BPH)]
| Anesthesia | Method | Treatment Duration | Hospital Stay Duration | Invasiveness | Insurance | |
| Prostatic Artery Embolization(PAE) | Local anesthesia | Embolization of the blood-supplying vessels through a catheter within the artery | 2hours | N/A | Low | Not covered by insurance |
| Transurethral Resection of the Prostate(TURP) | General or spinal anesthesia | Endoscopic resection of the prostate through the urethra | 2hours | 5days | Med | Covered by insurance |
| Holmium Laser Enucleation of the Prostate(HoLEP) | General or spinal anesthesia | Endoscopic enucleation of the prostate using a laser through the urethra | 2hours | 5days | Med | Covered by insurance |
FLOW
【Inquiry】
【Consultation & Diagnosis】
【Treatment Planning】
【Treatment】
【Follow-up】
2 Aortic Aneurysm The aorta enlarges, and if left untreated, it may rupture, posing a risk of death.

Minimally Invasive Aneurysm Treatment
Stent Graft Treatment (EVAR)
EndoVascular Aneurysm Repair
Normal Aorta
Aortic Aneurysm
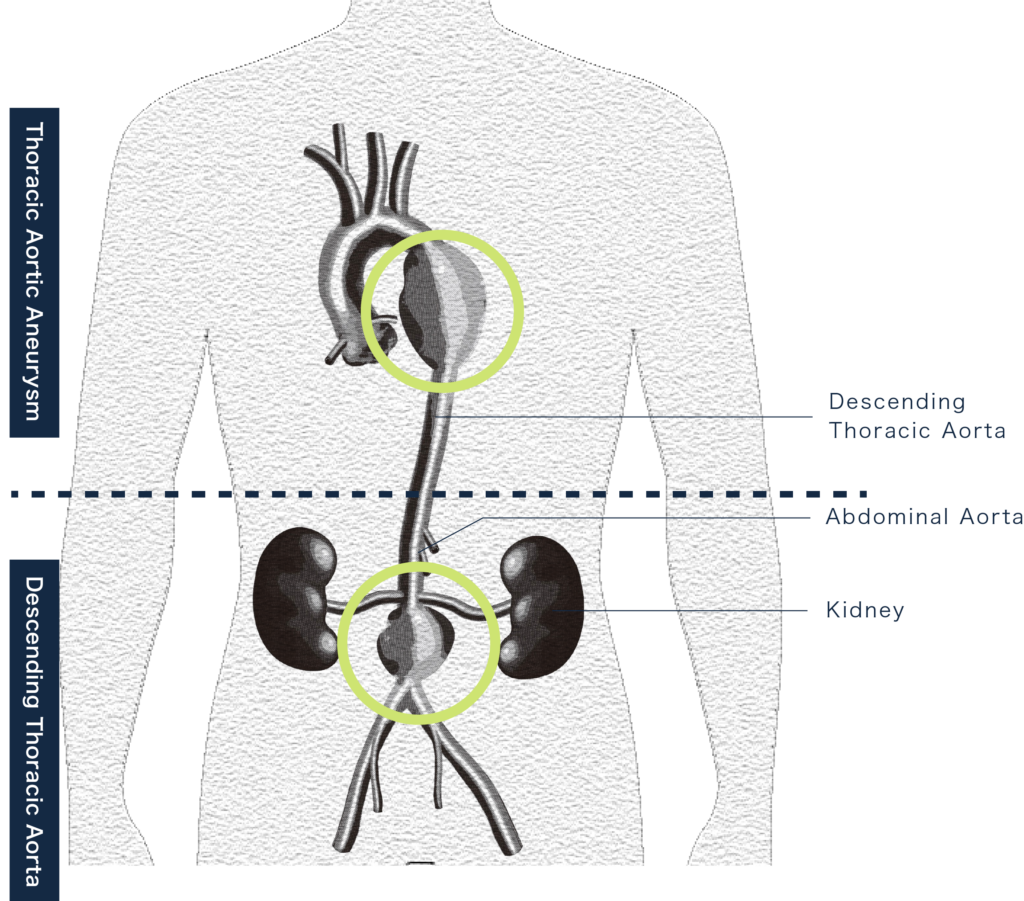
【Disease Overview】
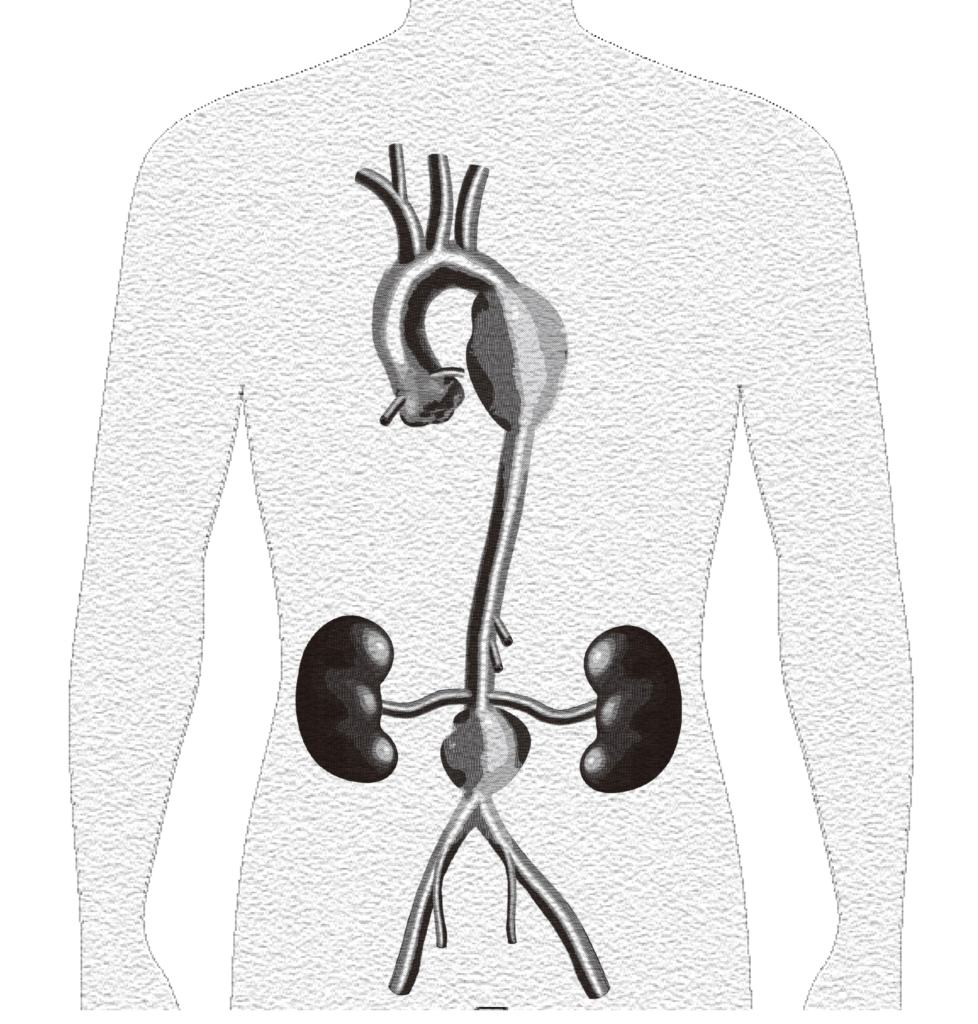
An aortic aneurysm is a condition in which the aorta swells like a bulge. It occurs in weakened areas of the arterial wall ( “the wall of the blood vessel”), and when subjected to blood flow pressure, it expands outward.If left untreated, the aneurysm can continue to enlarge, significantly increasing the risk of rupture and massive internal bleeding. Once an aneurysm ruptures, the prognosis is extremely poor. In some cases, patients may not even reach the hospital and suffer sudden death.The mortality rate for ruptured aneurysms is estimated to be as high as 60-80%.
【Main Symptoms】
Most aortic aneurysms are asymptomatic and gradually enlarge without the patient noticing. In some cases, when the aneurysm becomes significantly large, it may be detected due to abnormal pulsation in the abdomen or discovered incidentally during a medical check-up.If an aneurysm ruptures, it often causes severe pain in the back, lower back, or abdomen. The patient may rapidly go into shock, and without immediate treatment, death due to hemorrhage is inevitable.

Treatment
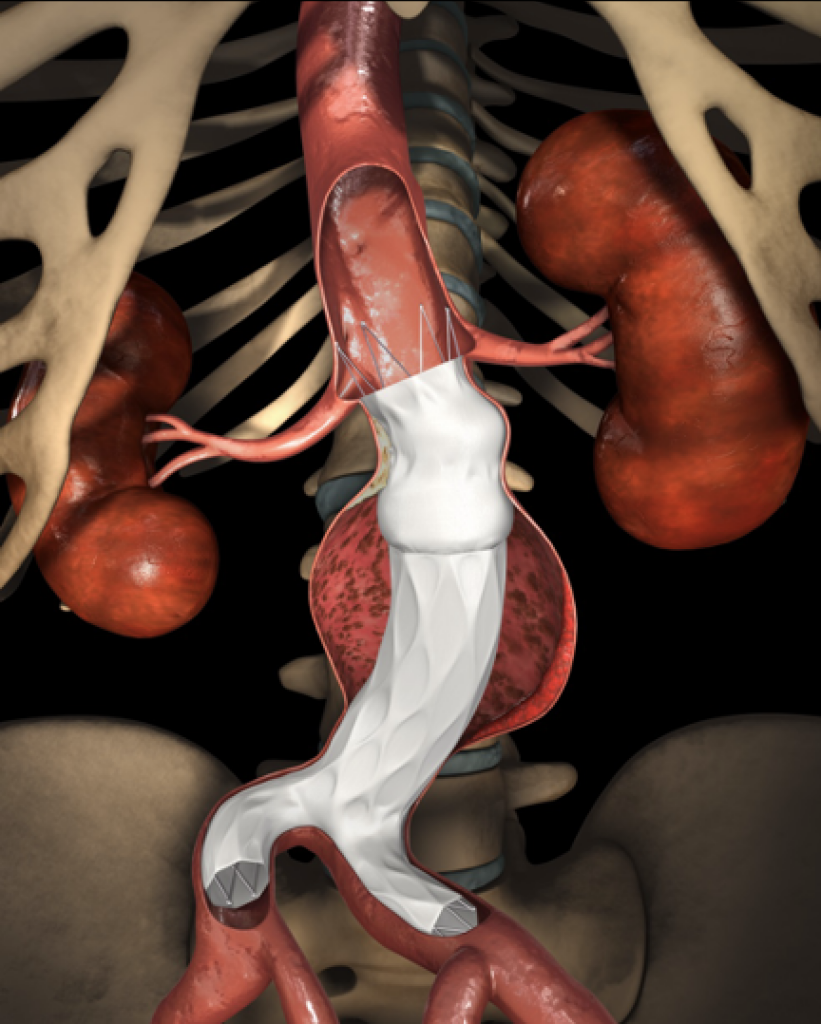
Minimally Invasive Treatment
Since 2007, commercially available stent grafts for abdominal aortic aneurysm (AAA) treatment have been covered by insurance in Japan, making them accessible for clinical use.A stent graft consists of a metallic framework called a stent and an artificial vascular graft that covers it. Unlike traditional open surgery, which requires opening the abdomen or chest, stent grafts are placed using a catheter inserted through the femoral artery in the groin.Once the stent graft is deployed in the aneurysm, it prevents direct blood pressure from affecting the weakened arterial wall, thereby eliminating the risk of rupture. Studies worldwide have reported excellent outcomes with this method.
Endovascular Aneurysm Repair (EVAR) is a minimally invasive vascular treatment, meaning it places less strain on the body compared to open surgery. One of its greatest advantages is that it can even be performed under local anesthesia.
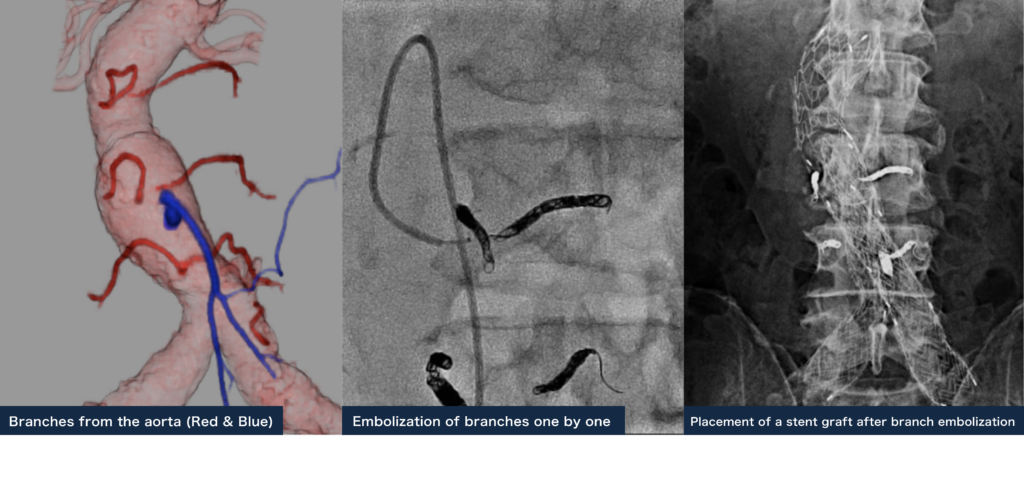
[Minimizing Complication Risks]
Compared to traditional open surgery, EVAR (Endovascular Aneurysm Repair) is a minimally invasive procedure, making it a safer option for elderly patients. However, some reports suggest that long-term outcomes beyond 10 years may be inferior to open surgery.One of the main reasons for this is type II endoleak, which occurs due to retrograde blood flow from aortic branches. Even when the aneurysm is covered with a stent graft, persistent blood flow into the aneurysm sac can lead to aneurysm growth if a type II endoleak develops. Studies have indicated that the risk of aneurysm rupture beyond 8 years post-surgery is higher with EVAR than with open surgery.To address this issue, preventive embolization of aortic branches is now commonly performed immediately before the stent graft placement to reduce the occurrence of type II endoleak and improve long-term outcomes.
FLOW
【Inquiry】
【Consultation & Diagnosis】
【Treatment Planning】
【Treatment】
【Follow-up】
3 Lower Extremity Arterial Disease (LEAD) Arterial occlusion in the lower limbs causes various symptoms.
Lower Extremity Arterial Disease
【Disease Overview】
Lower Extremity Arterial Disease is a condition in which arteriosclerosis causes the arteries in the lower limbs to become obstructed. A characteristic symptom is intermittent claudication, where walking even a short distance causes pain in the muscles of the buttocks, thighs, or calves, but the pain subsides with rest, allowing the patient to walk again.As the condition worsens, patients may experience persistent coldness and severe pain in their feet even at rest, sometimes leading to sleep disturbances due to unbearable pain. In severe cases, ulcers or gangrene may develop on the feet and fail to heal. Without prompt blood flow improvement, some patients may require limb amputation (critical limb ischemia).Many patients are initially diagnosed with lumbar conditions such as lumbar spondylosis or herniated discs, leading to the overlooked presence of lower limb arterial occlusion.Our team has extensive experience in endovascular treatment for lower limb arterial occlusions and boasts world-class treatment outcomes. We are committed to performing safe and effective revascularization procedures to help improve the quality of life for patients suffering from intermittent claudication or critical limb ischemia.

Treatment
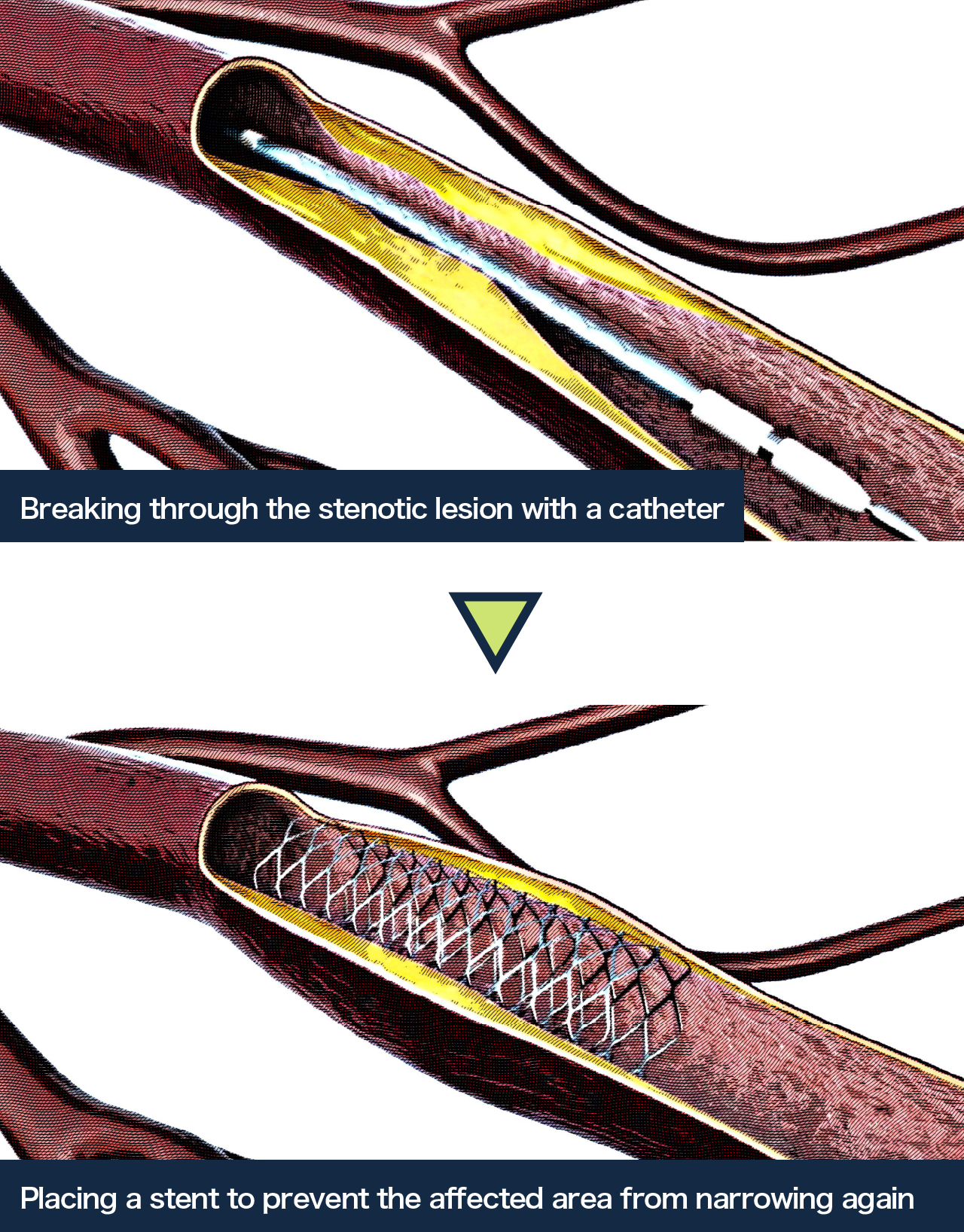
Endovascular Treatment for Lower Extremity Arterial Disease
Local anesthesia is administered, and a catheter is inserted into the blood vessel through a puncture in the groin or wrist artery. The narrowed section of the artery is expanded using a balloon, and in some cases, a stent is placed. Since all procedures are performed within the blood vessels, there is minimal pain, and the burden on the body is kept to a minimum. The treatment duration varies depending on the location and complexity of the procedure but generally takes around 30 minutes to 2 hours.
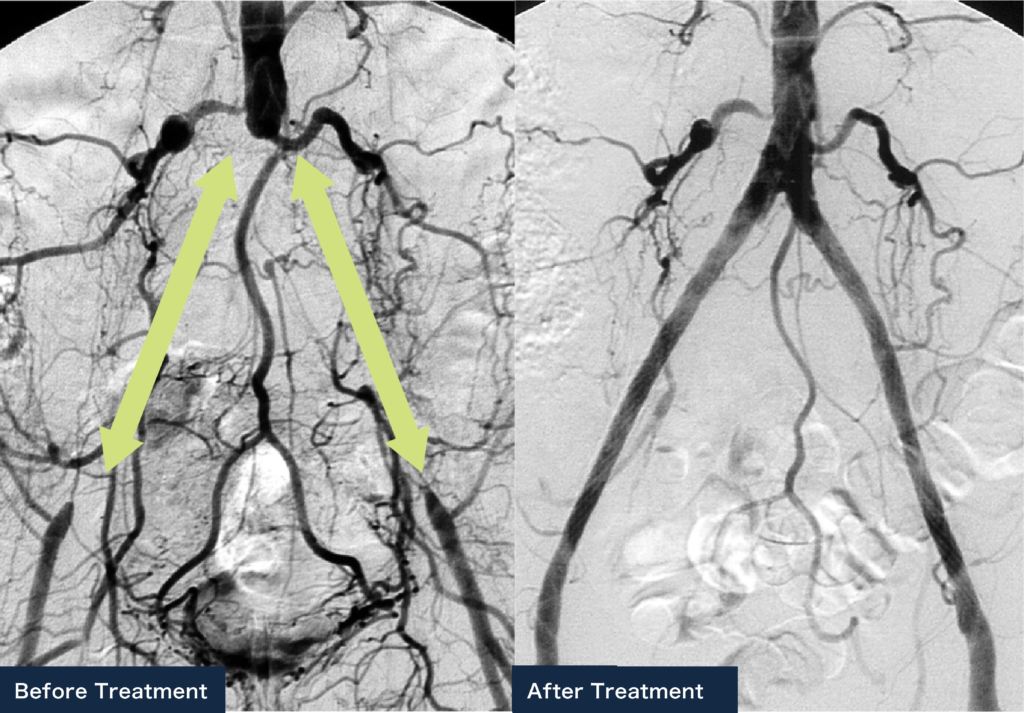
[Endovascular Treatment Outcomes for Lower Extremity Arterial Disease]
We have previously compiled the treatment outcomes of iliac artery stenting and published our findings in the Journal of Vascular Surgery in the United States¹. The patency rate of iliac artery stents (the probability that blood flow remains unobstructed after stent placement) was favorable, ranging from 71% to 83% over 10 years.Unlike surgical procedures, endovascular treatment allows for repeated interventions if a stent becomes occluded. When including cases where reintervention successfully restored blood flow, the 10-year patency rate of stents reached 98%.
[Endovascular treatment dramatically improves symptoms]
A patient with bilateral iliac artery occlusion was referred to us due to intermittent claudication, experiencing pain in both legs after walking 100 meters. Stents were placed in both iliac arteries, resulting in successful vascular expansion and restored blood flow.Following the procedure, the patient’s walking pain disappeared, and they were able to walk for kilometers without the need for rest.
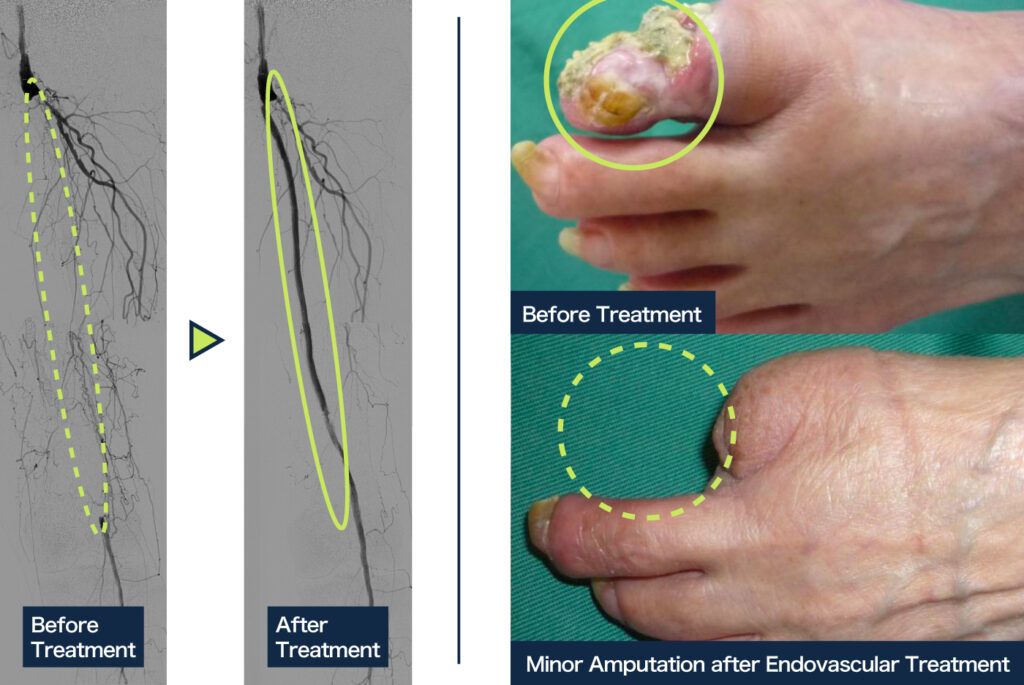
Another patient had necrosis in the left big toe and an occlusion in the left femoral artery. After placing a stent and performing revascularization, a minor amputation was carried out on the necrotic area. As a result, complete wound healing was achieved.
Reference:
Ichihashi S, Higashiura W, Kichikawa K et al. J Vasc Surg. 2011; 53: 992-9.
FLOW
【Inquiry】
【Consultation & Diagnosis】
【Treatment Planning】
【Treatment】
【 Follow-up】